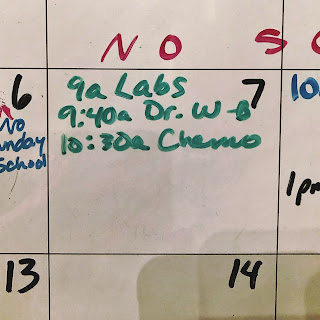
So we start the back half of treatment in the first week of the new year. And back to what I consider the normal schedule: 9:00 a.m. labs, 9:40 a.m. appointment with my oncologist, and chemo at 10:30 a.m.
Well, not quite normal. The cancer center was incredibly busy, I imagine partly due to the holidays and things were running behind.
My wife met me in the “small” exam room and we had a bit of a wait. I never mind as my oncologist is very attentive to all her patients. Anyway, it was probably about 10:15 or so before we met with my oncologist.
Fortunately my labs looked good and I didn’t have a lot of questions. My scans also came back good. Or really as good as they could be. No progression for the most part, and some mets have gotten smaller. But there are a LOT of mets. I asked how many there were and she really couldn’t quantify it as pretty much my whole spine was black in the scan, which means there are lots and lots of mets.
My previously swollen lymph nodes (only one or two) had shrunk and my prostate has been getting smaller too. That I can tell because peeing is a lot easier. Yeah, the Flowmax helps, but I can tell the difference with my prostate. One thing I didn’t get at my appointment was my PSA, as it wasn’t ready yet.
We made it to the third floor for chemo just a few minutes late. The waiting room was packed. I did have a longer wait than usual, but nothing outlandish. It was nice to just sit. I did some 4-7-8 breathing exercises and then just enjoyed the wait. Not too long and the pager buzzed and I was on my way in.
This time I got a room with a window. Normally that’s a good thing, but it was cold outside and the windows were drafty. Reminds of a time when I got a rental car that was a convertible, which I suppose is a good thing (despite being terrified of them), but it was December, bitter cold, and it was snowing.
I got my warm blanket and I was happy. The good news is the nurse who would be administering my chemo was this really nice (and very thorough) lady from Ethiopia who I’ve had before, I think during my first round. This is my 10th chemo and I didn’t start blogging about them until this time around so I’m not really sure.
There was some delay in getting the medicine from the pharmacy, so we didn’t get started until about 11:30, an hour later than scheduled. Not a big deal, I enjoyed just sitting. I asked for a sack lunch, but apparently there weren’t any. The Ethiopian nurse brought me some snacks, which was very kind of her. Some peanut butter crackers and a little pack of shortbread. And later she found a frozen peanut butter and jelly sandwich that I saved for later. And my wife brought some Tippins pumpkin pie. Not sure what it is about pumpkin pie and chemo, but for me, the two go hand in hand. My oncologist’s nurse called and let me know my PSA had gone down to 2.8! I can’t remember the last time it was under 3.
Another nurse came in to do the pre-chemo drip. When I mentioned the Benadryl just wiping me out, she said she would administer it to me in one-minute intervals over the course of five minutes. Ok, this nurse deserves an award of some kind. This made a huge difference. It took five or ten minutes before I even felt it. And I simply felt groggy, which is way better than falling asleep in a matter of seconds. I nodded of here and there, but I was with the world for the duration. And when we left I was cognizant and could walk out on my own two legs. Still, it’s 7:00 p.m. and I’m going to bed.